The current situation of the HIV/AIDS epidemic - 2013

The global situation
According to UNAIDS estimates for the year 2012, 35.3 million persons are infected with the HIV virus worldwide and there were 2.3 million new infections and 1.6 million deaths that year. Sub-Saharan Africa is by far the hardest-hit region, with 25 million people infected, followed by South and Southeast Asia, with a combined total of 4.8 million. The burden of the epidemic in a given country is expressed by the proportion of infected persons among the entire adult population, or prevalence. Prevalence varies greatly by country; the highest rates are in Southern Africa; in some Southern African countries over 20% of the adult population is infected.
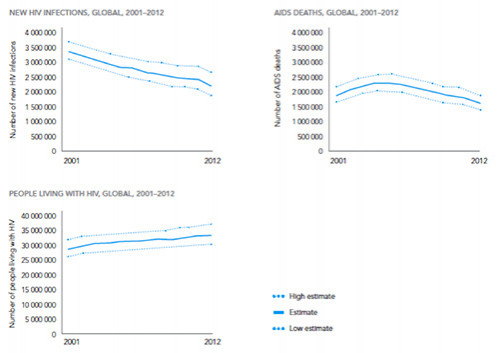
As shown by the graphs in Figure 1, the global epidemic has receded considerably in recent years. New infections are down 33% from 2001 and the number of deaths from AIDS has fallen 30% from the peak reached in 2005. Nonetheless, the number of persons living with HIV continues to rise, as a consequence of the number of new infections remaining higher than number of deaths.
Figure 1. Trends in the number of people living with HIV, new HIV infections, and AIDS deaths, global data for 2001-2012
The fall in new infections is due to a combination of several factors
Prevention efforts, particularly those focused on changes in sexual behavior, such as condom use, later sexual debut, and reducing the number of sexual partners, have played an important role in limiting new infections. The increase in number of infected persons receiving antiretroviral treatment has also been important in controlling sexual transmission of the virus (see below). In addition, male circumcision, now practiced in countries with extremely high prevalence rates where few men were circumcised traditionally, has proven effective in reducing woman-to-man transmission.
Generalised and concentrated epidemics: one type of epidemic may conceal another
For UNAIDS, an epidemic is "generalized" when HIV prevalence exceeds 1% of the general adult population (15-49 years of age). For situations where HIV prevalence in this population is under 1% but exceeds 5% in "vulnerable" sub-populations (e.g., sex workers, men who have sex with men, injecting drug users), UNAIDS uses the term "concentrated" epidemic. Since 2006, the term "hyper-endemic" has been applied to the epidemic in southern Africa, where prevalence exceeds 15%. According to these definitions, most countries in sub-Saharan Africa have generalized epidemics with coexisting "concentrated" epidemics.
Antiretrovirals: a revolution
Combinations of antiretroviral drugs (triple therapies or combination therapies) have been available since 1996. These treatments prevent virus multiplication and enable the immune system, whose cells are destroyed by the virus, to recover; the body can once again fight against infections. By dramatically reducing the morbidity and mortality associated with HIV, these treatments have transformed the infection into a chronic disease.
The demographic impact of antiretroviral treatment has been demonstrated with remarkable clarity in a rural zone of KwaZulu-Natal, South Africa, where more than one adult in five is HIV-infected. Life expectancy there has risen ten years since 2004, when the treatment access programme was first implemented. The impact of AIDS for the society has been considerably reduced: adults under treatment can return to work, raise their children, care for elderly parents. They face a new challenge, though: ageing with HIV. More than 10% of adults living with HIV in resource-limited settings are over 50 years of age.
Antiretrovirals also help contain the epidemic by reducing contamination risk for non-infected persons. An international clinical trial has shown a 96% fall in infection risk in serodiscordant couples where the infected member is undergoing treatment.
In recent years there has been a sharp increase in the number of persons with access to antiretrovirals: they totalled 10 million in 2012. This number corresponds to 65% of adults in need of treatment worldwide, but only 34% of children. The number of persons undergoing treatment should rise considerably in the coming years following the promotion of HIV testing as well as the new WHO recommendations calling for earlier treatment in the course of the disease.
Fewer and fewer children affected by HIV
The HIV virus may be transmitted sexually, by blood, or by mother-to-child transmission during pregnancy, birth, or breast-feeding. In ten years the number of new infections among children under 15 has been halved thanks to antiretroviral treatment of HIV-positive pregnant women, which considerably reduces mother-to-child HIV transmission. It is estimated that at the end of 2012 approximately 63% of HIV-positive pregnant women worldwide were receiving preventive treatment. A new strategy has been implemented in some high-prevalence countries: providing simple, lifelong antiretroviral treatment to all pregnant women who test positive for HIV, regardless of the stage of their disease. In addition to preventing transmission to the child during that pregnancy and any later ones, this strategy protects the mother’s health and reduces transmission to HIV-negative partners, therefore contributing to containing the epidemic. However, the effectiveness of this strategy depends on several factors, namely the ability of the health systems to implement and maintain the treatment programme over the long term and the ability of the HIV-positive women to continue the treatment throughout their lives.
New prevention issues
With regard to prevention through antiretroviral treatment, mathematical models suggest that with universal, repeated screening for HIV (to identify infected persons as early as possible) and immediate treatment for all HIV-positive persons, the epidemic could be overcome in 30 to 40 years’ time in such countries as South Africa. This strategy, known as "TasP" for Treatment as Prevention, is currently being assessed through clinical studies in southern Africa aimed to evaluate the benefits of such strategy at both the collective level (decrease in new infections) and individual level (improvement in the health of the persons undergoing treatment).
Another prevention strategy is pre-exposure treatment (PrEP: pre-exposure prophylaxis), which consists in treating HIV-negative persons either continuously or occasionally (for example, just before having potentially risky sex). Several trials are underway in this area, including IPERGAY in France.
Research into a vaccine had been under way for the last twenty years and continues, but all vaccine prototypes developed until now have proven to be either ineffective or only slightly effective.
A few cases in which the infection was controlled after interruption of treatment have raised hopes of a "cure", while until now, infected persons have been able to lead near-normal lives only at the cost of lifelong treatment. Several research studies are being conducted in this direction and they continue to suggest the effectiveness of starting treatment as soon as possible after contamination.
Now more than ever, prevention and treatment must not be dissociated. But individuals need to know their HIV status. Keeping the general public informed and providing broad access to screening, prevention methods, and treatment are the best means of containing the epidemic.
Contact: Joseph Larmarange (IRD, CEPED) and Sophie Le Coeur (INED)
Online: December 2013
